SMA President’s Message: January 2018
DONALD DIPETTE, MD, COLUMBIA, SOUTH CAROLINA
Dr. DiPette was installed as SMA’s 113th President during the 2nd General Session of SMA’s Medical Summit Conference, November 4, 2017 in St. Petersburg, Florida. His Presidential Address focused on key elements of the Association’s mission statement … quality, patient care, and education.
Dr. DiPette’s Message:
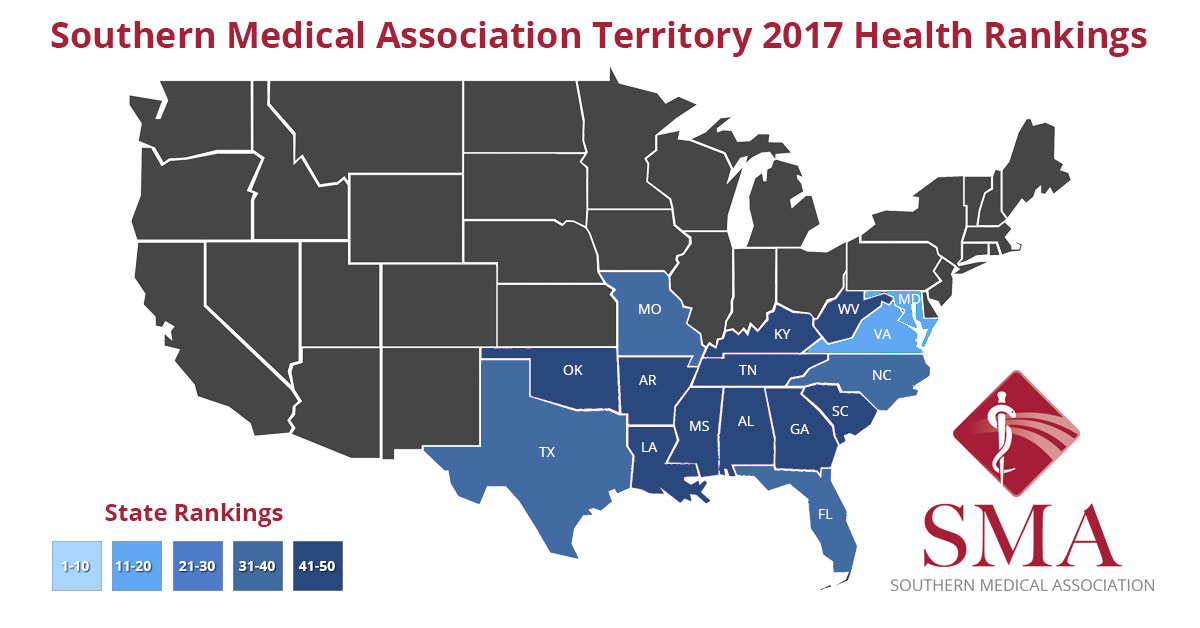
I hope everyone in the Southern Medical Association family had a wonderful holiday and I wish all a very Happy New Year! It is an honor to bring this first quarterly President’s Message of 2018 to you. I am grateful to be entrusted with the leadership of our Association and thank all the members and staff who commented positively on the content of my President’s Inaugural Address. This year is off to a running start, building on the planning and accomplishments of the last year. There is a great deal of excitement, energy, and enthusiasm and multiple new initiatives and programs are underway. This quarterly message will follow this year’s theme, “Addressing the Increased Disease Burden in the Southern Region”, as well as, the four areas for growth, namely, Relevance of our association, Collaboration with other organizations sharing similar and complementary missions and visions, Engaging academia and academic medical centers, and Develop and implement a youth strategy, which are detailed in the Presidential Address.
Despite the hectic holiday season, our new committees are well underway. The Education Committee, under the leadership of Dr. Christopher Morris, has developed an overall agenda for the year and is actively meeting and planning our Annual Scientific Assembly to be held in the fall. In addition, a new calendar of Web-based educational activities for the remainder of the year is being developed. The Membership Committee, chaired by Dr. Lee Carter, is actively seeking members and will meet in the near future. Although a seemingly “thankless” job, increasing membership is our life-line to the future. I encourage all members to consider joining and supporting the committee. The Health Policy Committee Chair position is currently vacant; if you are interested in either chairing this committee or serving on the Health Policy Committee or the Membership Committee, please contact Wendy Erhart at wendy@sma.org for more information. The Budget and Finance Committee, chaired by Dr. Gary Delaney, met during the Annual Meeting in November and will meet again this month. Thank you to all serving on these committees; your leadership, dedication, and commitment to the Association are invaluable.
To address this year’s theme of “Addressing the Increased Disease Burden in the Southern Region”, we have developed a partnership with Clinical Care Options to develop diabetes education programs in 10 cities across the South. The goal of this partnership is to improve participants’ clinical competence in preventing type 2 diabetes mellitus, and applying culturally competent treatment strategies in the management of patients with type 2 diabetes mellitus and associated cardiovascular risks.
To remain relevant in today’s healthcare environment, our Association must seek ways and methodologies targeted to increase the awareness and application of new technology which will enhance patient care in both the inpatient and outpatient settings. We are pleased to share our collaboration with Dr. Michael Wagner, Assistant Professor of Internal Medicine and Director of the Internal Medicine Ultrasound Education program at the University of South Carolina School of Medicine in Columbia, S.C., in developing a hands-on course for the 2018 Women’s Health Conference that focuses on handheld/portable ultrasound technology in primary care. Dr. Wagner also is guest editing a series of articles for the Southern Medical Journal related to the clinical use of portable ultrasonography.
It is critical that the SMA develops relationships, partnerships, and collaborations with organizations sharing similar and complementary missions and visions. We are pleased to announce that immediately following the 2018 Annual Scientific Assembly, the SMA will jointly sponsor with the Carolinas, Georgia & Florida Chapter of the American Society of Hypertension and the World Hypertension League, a one-day symposium focusing on hypertension, stroke, and cardiovascular disease. In addition, the SMA has served as the accrediting provider for the recent Society of Gynecologic Surgeons’ postgraduate course, as well as for the Society’s upcoming annual meeting.
Planning of this year’s Annual Meeting is underway, and to reach out and engage academia, we are currently developing a Deans’ Forum that will take place at the opening of the Assembly on October 31, 2018. Designed to include the deans or their designees from the four medical schools in South Carolina, the purpose of this panel discussion is twofold: to discuss academia’s collaborative role with associations such as SMA and to address the role academia plays in addressing the SMA’s theme, “Addressing the Increased Disease Burden in the Southern Region”. In addition, the forum will provide an opportunity to highlight activities of the respective medical schools and their associated healthcare systems.
The SMA has a long, rich tradition of developing physician leaders in medicine. This development must start very early in the future and present careers of our younger learners and physicians. In keeping with this “Youth Movement”, greater emphasis has been placed on expanding opportunities for Medical Students, Residents, and Fellows to be involved in our association. Such opportunities include presenting to and becoming more involved in the annual assembly, and in the future, to ultimately lead SMA. The Annual Assembly this year will dedicate a day to young physician education and leadership. Tentative activities being planned include additional time for poster presentations and oral abstracts, as well as a roundtable luncheon with academic and association leadership. Information will be online soon -- please visit sma.org/assembly in the coming few weeks for the latest on topics and events!
As can be seen from the activities detailed above, this year is off to a running start! It goes without saying, this could not be accomplished without the participation of a dedicated membership and staff.
Again, I extend my heartfelt thanks; it is a privilege to serve as your President. Please feel free to contact the SMA headquarters office or me with your ideas, thoughts, and comments. Together, we can achieve great things!
Sincerely,
Donald DiPette, MD, FACP, FAHA
SMA President, 2017-2018
Email: ddipette@sma.org


















 Editor’s Note:
Editor’s Note: