Beyond the Stethoscope: Why Point-of-Care Ultrasound is a Game-Changer for Primary Care
It's 10:30 a.m. on a busy Thursday in your primary care clinic. Mrs. Smith, a 52-year-old patient, arrives for a sick visit. She has been having a cough, fatigue, and mild shortness of breath for 5 days. She did have a sore throat and rhinorrhea preceding her symptoms. Her oxygen saturation is 94%, and you hear coarse breath sounds on the right. You wonder if she has a vira
l infection or a bacterial pneumonia that requires antibiotics. You’d normally send her out for a chest X-ray, but instead, you reach for your point-of-care ultrasound (POCUS) device.
Figure 1 shows the patient’s right lung base. What do you see?

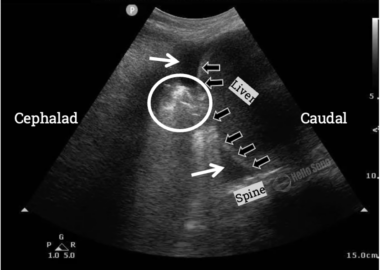
Notice the presence of a spine sign, visualization of the spine superior to the diaphragm (black arrows).
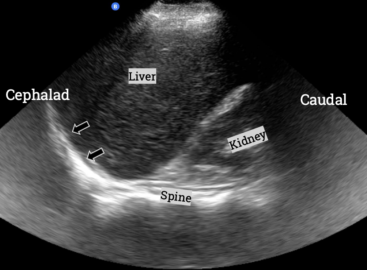
Figure 2 shows a normal right lung base from a different patient.
Within a few minutes, you visualize a consolidation in the right lower lobe that confirms your suspicion of a bacterial pneumonia. You start her on appropriate antibiotics, thus saving time, reducing costs, and avoiding unnecessary radiation. You also show Ms. Smith exactly what’s going on in her lungs, and she walks away fully committed to taking her medications as prescribed.
This case highlights how POCUS can revolutionize diagnostics in primary care settings, providing real-time, actionable insights at the bedside. While this technology has been used in emergency medicine for over two decades, it's now increasingly making its way into primary care due to its proven benefits.
Why Now is the Time for POCUS in Primary Care
Affordability: POCUS devices have become significantly more cost-effective. Handheld units now range from $2,000 to $10,000, compared to traditional cart-based systems that used to cost over $20,000.
Evidence-Based: POCUS is supported by robust clinical evidence demonstrating improved diagnostic accuracy, expedited care, and better patient outcomes. It is endorsed by multiple medical organizations as being within the scope of practice for primary care providers.
Value-Based Care: POCUS aligns with value-based care initiatives, reducing unnecessary referrals and imaging, and improving diagnosis accuracy. This translates into reduced healthcare costs and improved patient outcomes.
Addressing Workforce Shortages: With shortages of ultrasound and radiology technicians, POCUS offers a convenient, in-house solution for primary care providers.
Revenue and Patient Engagement: In a time when many practices are seeing decreased patient volumes and stagnant reimbursements, adding services like POCUS can attract new patients, increase patient satisfaction, and generate additional revenue.
Common Primary Care Scenarios That Benefit from POCUS
- Soft Tissue Infections: POCUS excels in evaluating cellulitis and abscesses, distinguishing between the two when the physical exam is uncertain. This prevents unnecessary incisions, reduces antibiotic misuse, and saves patient discomfort. [1-3]
- Respiratory Complaints: Lung POCUS can detect pneumonia, pleural effusions, pulmonary edema, and pneumothorax with greater sensitivity than chest Xray. It’s especially useful for children, pregnant women, and patients at higher risk from radiation exposure. In addition, focused cardiac ultrasound can rapidly screen for pericardial effusion and reduced systolic function.
- Abdominal Pain: Biliary and renal POCUS can efficiently evaluate patients with abdominal pain, detecting conditions like cholecystitis, nephrolithiasis, and hydronephrosis, which can prevent unnecessary CT scans. Plus, POCUS can be used for screening for abdominal aortic aneurysms in male smokers over 65 years old.
- Musculoskeletal Pain: Assessing joint effusions, tendonitis, tendon ruptures, fractures, and even dislocations is possible with POCUS, providing immediate guidance for management.
- Lower Extremity Pain or Swelling: POCUS can be employed to exclude proximal leg deep venous thrombosis (DVT) using a compression technique, preventing unnecessary emergency department referrals. [8,9]
- Procedural Guidance: Using POCUS for procedures like joint injections, abscess drainage, or difficult IV access improves both success rates and patient comfort.
How POCUS Benefits Your Practice
POCUS does more than enhance patient care; it can also improve your clinic's bottom line by:
- Boosting patient satisfaction through faster diagnosis and treatment.
- Increasing adherence to follow-up imaging when patients see the results firsthand.
- Expanding your service offerings to attract new patients.
- Allowing for in-house imaging capabilities, reducing referrals, and enhancing revenue potential.
In Conclusion
POCUS is a game-changer for primary care providers, enhancing diagnostic accuracy, reducing costs, and improving patient outcomes. With devices now more affordable than ever and training readily accessible, it’s time for primary care practices to integrate POCUS into their diagnostic toolkit. This technology empowers providers to deliver high-quality care that aligns with value-based care principles, ultimately leading to better patient satisfaction and financial performance.
References
- Tayal VS, Hasan N, Norton HJ, Tomaszewski CA. The effect of soft-tissue ultrasound on the management of cellulitis in the emergency department. Acad Emerg Med. 2006;13(4):384-388. doi:10.1197/j.aem.2005.11.074
- Costantino TG, Satz WA, Dehnkamp W, Goett H. Randomized trial comparing intraoral ultrasound to landmark-based needle aspiration in patients with suspected peritonsillar abscess. Acad Emerg Med. 2012;19(6):626-631. doi:10.1111/j.1553-2712.2012.01380
- Rehrer M, Mantuani D, Nagdev A. Identification of peritonsillar abscess by transcutaneous cervical ultrasound. Am J Emerg Med. 2013;31(1):267.e1-267.e2673. doi:10.1016/j.ajem.2012.04.021
- Ticinesi A, Lauretani F, Nouvenne A, Mori G, Chiussi G, Maggio M, Meschi T. Lung ultrasound and chest x-ray for detecting pneumonia in an acute geriatric ward. Medicine (Baltimore). 2016 Jul;95(27):e4153. doi: 10.1097/MD.0000000000004153. PMID: 27399134; PMCID: PMC5058863.
- Pirozzi C, Numis FG, Pagano A, Melillo P, Copetti R, Schiraldi F. Immediate versus delayed integrated point-of-care-ultrasonography to manage acute dyspnea in the emergency department. Crit Ultrasound J. 2014;6(1):5. Published 2014 Apr 27. doi:10.1186/2036-7902-6-5
- Baid H, Vempalli N, Kumar S, et al. Point of care ultrasound as initial diagnostic tool in acute dyspnea patients in the emergency department of a tertiary care center: diagnostic accuracy study. Int J Emerg Med. 2022;15(1):27. Published 2022 Jun 13. doi:10.1186/s12245-022-00430-8
- Adhikari S, Amini R, Stolz L, et al. Implementation of a novel point-of-care ultrasound billing and reimbursement program: fiscal impact. Am J Emerg Med. 2014;32(6):592-595. doi:10.1016/j.ajem.2014.02.051
- Mumoli N, Vitale J, Giorgi-Pierfranceschi M, et al. General Practitioner-Performed Compression Ultrasonography for Diagnosis of Deep Vein Thrombosis of the Leg: A Multicenter, Prospective Cohort Study. Ann Fam Med. 2017;15(6):535-539. doi:10.1370/afm.2109
- Hannula O, Vanninen R, Rautiainen S, Mattila K, Hyppölä H. Teaching limited compression ultrasound to general practitioners reduces referrals of suspected DVT to a hospital: a retrospective cross-sectional study. Ultrasound J. 2021;13(1):1. Published 2021 Feb 2. doi:10.1186/s13089-021-00204-y
- Andersen CA, Brodersen J, Rudbæk TR, Jensen MB. Patients' experiences of the use of point-of-care ultrasound in general practice - a cross-sectional study. BMC Fam Pract. 2021;22(1):116. Published 2021 Jun 18. doi:10.1186/s12875-021-01459
About the Author
Dr. Havryliuk is an emergency physician with over 15 years of clinical point-of-care ultrasound (POCUS) experience, a past Emergency Ultrasound Director at Brooklyn Hospital in NY, and the founder of Hello Sono. She is on a mission to empower clinicians with POCUS to take better and more efficient care of their patients by addressing two key barriers, lack of competency and infrastructure.
LinkedIn: https://www.linkedin.com/in/tatiana-havryliuk-md/
Email: [email protected]
*POCUS images provided courtesy of Hello Sono.
